Blog
Go to the Next Level with 5-Part Differential Hematology Analyzers
A complete blood count (CBC) is typically the first test requested by a physician to evaluate a patient’s general health. Automated hematology analyzers are frequently used in physician office laboratories, small standalone labs and clinics for CBC screenings. Laboratories with low-volume solutions typically rely on 3-part differential hematology analyzers. However, older 3-part differential technology maybe holding busy laboratories back and trends show there is growing interest in 5-part differential hematology analyzers.
3-part Vs. 5-part Differential Hematology Analyzers
A 3-part hematology instrument provides enough information for typical physician office laboratories. With a simple CBC, the neutrophil and lymphocyte counts will answer the question of a viral infection or a bacterial infection that can be treated with antibiotics.
A 5-part differential hematology instrument uses the principle of flow cytometry to differentiate white blood cells (WBC) into their five major sub-populations—neutrophils, lymphocytes, monocytes, eosinophils, and basophils—based on cell size and complexity (granularity).
For specialty laboratories, a 5-part hematology instrument can provide a more detailed and targeted assessment of the blood status. To distinguish eosinophils and basophils from neutrophils, for example, a 5-part differentiation is necessary.
Improving Workflow Efficiency
The most important aspect of automated hematology analyzers is the ability of the analyzer to detect and flag for abnormal samples. Workflow efficiencies can be gained by significantly reducing suspicious flagging and the number of manual differentials. The number of samples that require manual examination can be greatly reduced with more detailed information and improved accuracy1,2 provided by a 5-part differential.
About 30% of samples generate a suspicious flag with a 3-part analyzer requiring a manual differential. The more detailed information provided by a 5-part differential analyzer can reduce suspicious flagging by about 10%.1
Improved Accuracy with Dynamic Gating Technology
Dynamic Gating Technologies achieve a high level of accuracy in the differential and are only available on 5-part differential hematology analyzers. The sophisticated gating technology improves identification of cell populations by adjusting the thresholds between cell cluster arrangements. In contrast, fixed gating technologies sometimes cause cells to be counted as part of an incorrect subtype, especially in pathological specimens generating suspicious flags.3
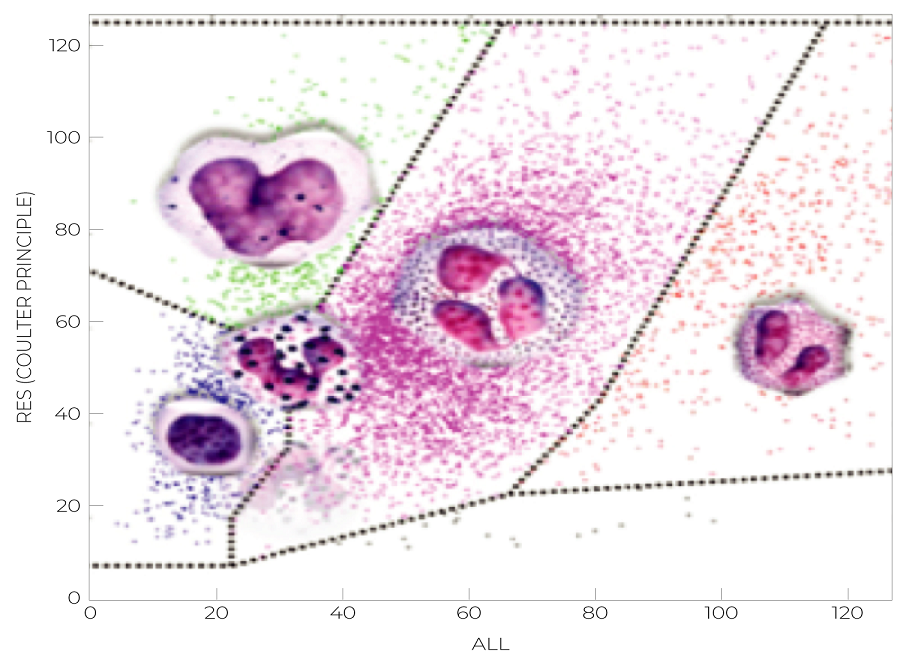
Image 2: DxH 500 Series Dynamic Gating 5-part Diff
Clinical Benefits for the Evaluation of Critical Parameters
Appropriate use of critical values improves patient outcomes by ensuring that physicians are promptly notified of immediate life-threatening conditions.5 For example, severe Neutropenia with critically low Absolute Neutrophil Count (ANC) below 500/μL is considered a critical parameter that cannot be overseen by clinicians. Proper evaluation and interpretation of critical Neutropenia requires an accurate Neutrophil count that cannot be achieved with a 3-part differential hematology analyzer. See (Table 1).5,6

Table 1: 3 and 5-part differential cell subtyping
5-part differential analyzers provide quantitative and qualitative measurements to differentiate and provide absolute counts for Basophils, Monocytes and Eosinophils. Measuring increased or decreased levels of WBCs can help distinguish abnormal samples from patients which may require further testing to determine if other conditions or diseases are present. 5-part differential analyzers provide important clinical information that is not attainable with a 3-part differential analyzer and can be used in identifying various clinically significant conditions like autoimmune diseases and infections.
5-Part Differential Hematology Solutions for Low-Volume Laboratories
The DxH 500 Series 5-part differential analyzers go beyond just cell counting. They provide the technological means for the identification of qualitative cell morphological characteristics to differentiate between normal and pathological conditions, improving the information provided to clinicians with 21 clinical parameters and improving laboratory workflow through reduction in suspicious flagging and increased accuracy. 5-Part differential hematology solutions maximize productivity in low-volume labs with 99% uptime.4

Interested in improving workflow efficiency in your lab? Learn how the DxH 500 Series hematology analyzers maximize productivity. Watch the video
Sources:
1. https://boule.com/content/uploads/2021/03/whitepaper-3p-or-5p-hematology-analyzers-31183-2.pdf
2. Noriyuki Tatsumi*, Izumi Tsuda*, Takayuki Takubo*, Masayuki Hino* “Practical Use of Automated White Cell Differential Analysis” *Osaka City University Medical School
3. DxH-500-Series-Dynamic-Gating-Technology-DS-111400-EN-GLB-A4
4. 2019-5865 DxH 520 Claims Matrix
5. Kenneth Emancipator, MD, Critical Values: ASCP Practice Parameter, American Journal of Clinical Pathology, Volume 108, Issue 3, 1 September 1997, Pages 247–253
6. http://ashpublications.org/hematology/article-pdf/2012/1/174/1501776/bep00112000174.pdf
7. LYRAD K. RILEY, MD, and JEDDA RUPERT, MD “Evaluation of Patients with Leukocytosis” AAFP December 1, 2015. Volume 92, Number 11

